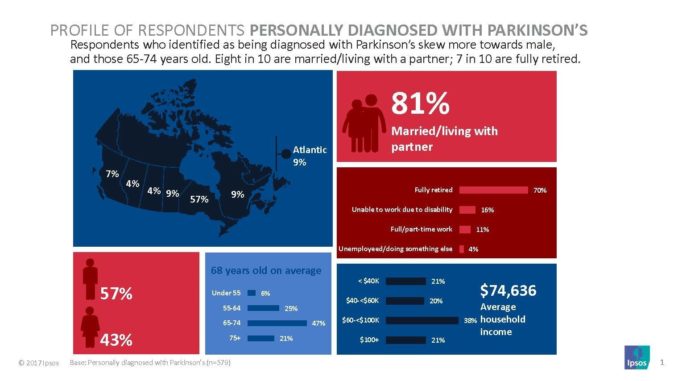
TORONTO, March 28, 2018 /CNW/ – Parkinson Canada, the definitive voice of the Parkinson community in Canada for over 50 years, recently conducted a survey through Ipsos Public Affairs, to better understand the challenges faced by three stakeholder groups:
- Individuals diagnosed with Parkinson’s disease
- Those who personally provide care to someone living with Parkinson’s
- Health care providers and those who work with people with Parkinson’s or with care partners.
Findings confirm what Canadians living with Parkinson’s along with their caregivers and health care providers have faced for some time. Access to specialized Parkinson’s care is often not available in a timely fashion. Other health services that improve the quality of life for both patients and caregivers can be limited.
“People with Parkinson’s often suffer from complex physical and non-motor health disorders, which can affect the whole family. We know that caregivers are heavily burdened, financially and emotionally. Our mission is to help close the gap for them and build awareness of Parkinson’s disease,” says Joyce Gordon, CEO of Parkinson Canada.
Survey Highlights
- Limited access and long wait times: 2 out of 10 waited more than one year for a diagnosis; 3 in 5 came to Parkinson Canada or one of its support groups, for additional information.
- Caregivers are burdened: more than 1 in 4 caregivers have full-time jobs while taking care of a loved one; 4 in 5 are married or living with their partner.
- Mental health: 4 in 10 or more people surveyed with Parkinson’s report experiencing depression, anxiety, stress, and loss of confidence.
- Financial burden: 4 in 10 agree that it is difficult to pay for health care bills relating to Parkinson’s disease, like medication, exercise, physiotherapy, and specialized services such as speech therapy.
“It’s important that individuals receive a correct diagnosis as early as possible and have adequate access to ongoing specialized care. Even this care is limited and follow-up visits are too far apart,” adds Dr. David Grimes, lead author of the Canadian Guidelines on Parkinson’s Disease and Head, Division of Neurology, The Ottawa Hospital. “If the survey shows that Canadians are experiencing considerable gaps and delays to care, this hinders health care professionals from effectively recommending treatments and lifestyle changes that would help patients better manage the disease.”
During Parkinson Awareness Month in April, Parkinson Canada will share the results with governments and other stakeholders, in order to raise awareness of these gaps in care. The organization will continue to advocate for improved access and reduced wait times. The organization will further share these results with the general public and donors, to seek more support. Additional investment is needed for exceptional research, to provide programs and services for people living with Parkinson’s, and to provide educational opportunities and resources for health care professionals.
With more than 25 people newly diagnosed each day in Canada, the demand for Parkinson Canada services and those of the health care system are increasing dramatically. It is critical that new investments be made now to expand services that ensure those living with Parkinson’s and their families, can live their best life possible. And research efforts must continue to increase our knowledge, improve treatments, and ultimately find a cure for this devastating disease.
Limited Access and Long Wait Times
Issues with access and wait times begin with obtaining a formal Parkinson’s diagnosis, requiring assessment by a neurologist or movement disorders specialist. Three out of 10 people waited more than six months for a diagnosis after first reporting their symptoms to a medical professional. Almost two out of 10 waited more than a year for a diagnosis. Nearly one in four people living with Parkinson’s rated access to medical specialists as poor or very poor, and a greater number also find access to movement disorder clinics or a Parkinson’s nurse specialist poor or very poor, with four in 10 currently a patient and one in 10 having been one in the past.
People living with Parkinson’s rate physical activity programs, physiotherapy and regular appointments with specialists, as services that would be most helpful to them. These two services are ranked highly among caregivers as well.
Four in 10 people living with Parkinson’s find access to long-term care facilities poor or very poor. On the other end of the access spectrum, nearly nine out of 10 rated access to oral medication good, very good or excellent and eight out of ten also rated access to a family doctor as good, very good or excellent.
In general, health care providers (HCPs) rated access to services and treatments more critically than those living with Parkinson’s and their care partners. In particular, more than half rated access to movement disorder clinics as poor or very poor; over four in 10 rated access to Parkinson’s nurse specialists as poor or very poor. Access to speech language and swallowing therapy, was also rated poor or very poor by nearly three in 10 HCPs.
Wait times for services and treatments were rated even more negatively than access by HCPs. Four in 10 or more rated wait times as poor or very poor for: long-term care facilities, access to therapies at all stages of the disease, medical specialists, Parkinson’s nurse specialists, and movement disorder clinics.
One in five HCPs surveyed cited a lack of medical specialists as one of the biggest barriers to people living with Parkinson’s getting the care they needed. Other barriers they noted include: more information and a better understanding of Parkinson’s, the availability of education resources and a lack of support groups or counselling.
Caregiver Burden
Among caregivers, almost half rated access to long-term care facilities poor or very poor. They also find access to movement disorder clinics and Parkinson’s nurse specialists limited. Similar to responses from those they care for, most caregivers find access to oral medication and their family doctor good, very good or excellent.
Nearly three in 10 caregivers find access to mental health services poor or very poor and nearly four in 10 find the wait times for these services poor or very poor.
One in four caregivers is working in a full-time job while caring for a partner with Parkinson’s. Three in four are female and one in four is over 75 years old.
Mental Health
People living with Parkinson’s reported experiencing depression, anxiety, stress, loss of confidence and sadness. Caregivers also reported often feeling stressed, exhausted and guilty they aren’t doing enough; one in four works full-time. Additionally, six in 10 or more reported feeling frustration towards the person with Parkinson’s; helpless and anxious at least some of the time; with about two in 10 reporting feeling this way often. One in five people living with Parkinson’s find access to mental health services poor to very poor, and nearly three in 10, find wait times for such services poor or very poor.
Nearly six in 10 health care providers rated access to mental health services as poor to very poor and the same number found wait times for these services as poor or very poor.
Financial Burden
Medication, exercise and physiotherapy are the most common services/treatments used by people living with Parkinson’s, with additional services added as the disease progresses, such as speech language and swallowing therapy, occupational therapy and consultations with dieticians.
Three quarters of people living with Parkinson’s and their care partners report paying out of pocket for exercise programs and 44 percent pay for physiotherapy themselves. More than a third pay for some medication out of pocket. Without reimbursement by insurers (public or private) four out of 10 would find paying for medication a major financial burden and almost the same number would find paying for other treatments a major burden.
Compared to those with Parkinson’s and caregivers, HCPs were more likely to see medication and other treatments for Parkinson’s as a financial burden, if they were not reimbursed by private insurance, or covered by provincial health programs. Three out of four thought the costs of treatments such as physiotherapy, occupational therapy, counselling, speech and other therapies, would be a major financial burden for patients if not covered. Three out of five think medication costs would be a major burden.
Survey Methodology and Credibility
A 30-minute online survey was conducted between September 29 and October 24, 2017. A link provided by Ipsos to the survey was sent out to 25,853 stakeholders by Parkinson Canada with two reminder invites. The margin of error for the total sample of 1,478 is plus or minus 2.5 percentage points, 95 percent of the time.
To view a summary of the survey, visit https://www.ipsos.com/en-ca/news-polls/Parkinson-Canada-stakeholder-survey-2018.
About Parkinson Canada
Parkinson Canada provides services and education to support people living with Parkinson’s disease, their families, and the health care professionals who treat them. Operating since 1965, the organization advocates on issues that concern the Parkinson’s community in Canada. The Parkinson Canada Research Program funds innovative research for better treatments and a cure.
A national registered charity, Parkinson Canada fulfils its mission through the generosity of donors and is an accredited organization under the Imagine Canada Standards Program. Parkinson Canada participates in numerous coalitions and partnerships to effectively fulfil its mission.
- Parkinson Canada is a founding member of Neurological Health Charities Canada (NHCC), whose primary aim is to seek a national brain strategy. In partnership with the Public Health Agency of Canada, a national epidemiological study of neurological disease was published in 2014.
- Parkinson Canada cooperates with a vast range of international, provincial or locally based organizations, whenever it advances the cause of the Parkinson’s community.
- Parkinson Canada is a member of the Best Medicines Coalition, Carers Canada, Canadian Coalition for Genetic Fairness, Health Charities Coalition of Canada and the World Parkinson Coalition.
SOURCE Parkinson Canada

CONTACT: and to arrange an interview, contact: Marina Joseph, Director, Communication and Brand, Parkinson Canada, 1-800-565-3000 ext. 3399, 416-227-3399, marina.joseph@parkinson.ca
RELATED LINKS
http://www.parkinson.ca
Leave a Reply